If you have found us early in your journey, we want to provide some more information on what a NICU experience might look like for you and your child.
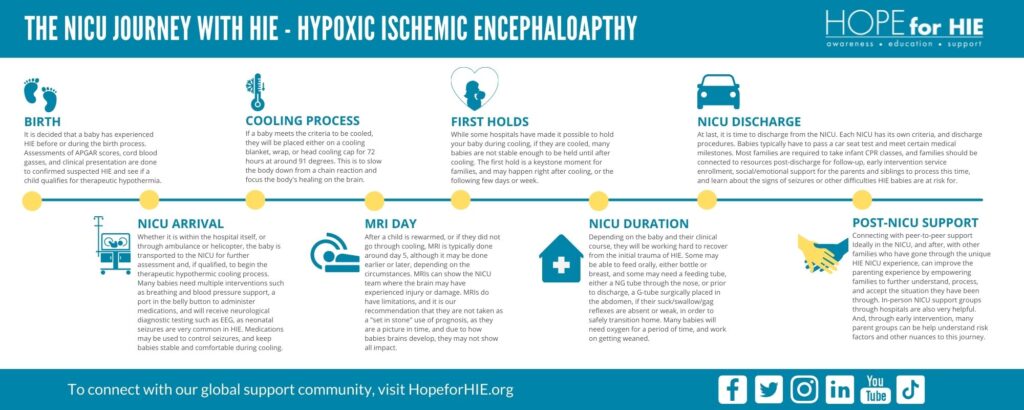

A baby is born – they may have experienced HIE before or during the birth process. Assessments of APGAR scores, cord blood gases, and a baby’s situation are done to confirm suspected HIE, and to see if a child qualifies for therapeutic hypothermia (cooling).

Whether it is within the birth hospital, or through ambulance or helicopter, the baby is transported to the NICU for further assessment and, if appropriate, to begin the therapeutic hypothermic cooling process. Many babies need multiple interventions such as breathing and blood pressure support, an IV in the belly button to administer medications, and will receive neurological diagnostic testing such as EEG, as neonatal seizures are very common in HIE. Medications may be used to control seizures, and keep babies stable and comfortable during cooling. Many hospitals have access to mental health resources in the NICU for families, so be sure to connect with the social worker.
If a baby meets the criteria to be cooled, they will be placed either on a cooling blanket, wrap, or head cooling cap for 72 hours at around 91⁰F. This is to slow the body down and focus the body’s healing on the brain. If you are unable to hold your baby during cooling, talk to your team about other ways to make memories, bond and care for your baby during this part of the journey.

After a child is rewarmed, or if they did not go through cooling, a MRI is typically done around day 5, although it may be done earlier or later, depending on the circumstances. MRIs can show the NICU team where the brain may have experienced injury or damage. MRIs do have limitations, and it is our recommendation that they are not taken as a “set in stone” use of prognosis. As they are a picture in time, and due to how babies brains develop, they may not show all impact. HIE has a wide range of outcomes.

While some hospitals have made it possible to hold your baby during cooling, if they are cooled, many babies are not stable enough. The first hold is a keystone moment for families, and may happen right after cooling, or the following few days or week, depending on the medical stability and touch tolerance of each baby.

Depending on the baby and their clinical course, they will be working hard to recover from the initial trauma of HIE. Families should be encouraged to attend daily rounds with the team. Some babies may be able to feed at the breast or using a bottle, and some may need a feeding tube placed through the nose to the stomach. If a baby’s suck/swallow/gag reflexes are absent or weak, a g-tube can be surgically placed in the abdomen, and allow the baby to safely transition home. Many babies will need supplemental oxygen for a period of time, and work on decreasing their need over time.

At last, it is time to discharge from the NICU. Each NICU has its own criteria, and discharge procedures. Babies typically have to be able to get safe and consistent nutrition whether by breast, bottle or tube, and meet other medical milestones. Most families are required to take infant CPR classes, and families should be connected to follow up primary and specialist care appointments, early intervention services, social/emotional support for the family to process this time, and learn about the signs of seizures or other difficulties HIE babies are at risk for.

Connecting with peer-to-peer support, ideally in the NICU, or after the baby goes home can improve mental health and the parenting experience. Connecting with other families who have gone through the unique HIE NICU experience can empower parents to further understand, process, and accept the situation they have been through. In-person NICU support groups through hospitals are also very helpful. And, through early intervention, many parent groups can be helpful to understand risk factors and other nuances to this journey.
Connect with families, read inspiring stories, and get helpful resources delivered right to your inbox.