Hypoxic (Lack of Oxygen)
Ischemic (Restricting Bloodflow)
Encephalopathy (Affecting the Brain)
When the brain is deprived of oxygen, brain cells are injured. Some may recover, some may die. The most common causes of oxygen deprivation to the brain are low levels of oxygen in the blood or a reduced flow of oxygen to the brain. This can happen in a variety of ways prior to birth, during the birth process, after birth, and during childhood. Hypoxic Ischemic Encephalopathy in the neonatal period falls under the umbrella of Neonatal Encephalopathy. HIE is the top cause of NE, and is also the top cause of neonatal seizures, although not all babies with HIE will experience seizures.
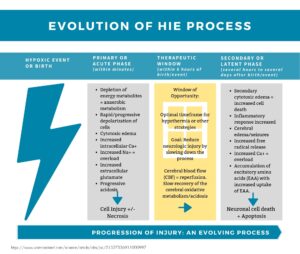
There are two stages of injury with HIE: The first stage happens immediately after the initial oxygen deprivation. The second occurs as normal oxygenated blood flow resumes to the brain. This is called “reperfusion injury” and occurs as toxins are released from the damaged cells. The “window of opportunity” is when interventions have been shown to decrease death and disability. However, we also know there are many children who fall outside of the “standard”, and may appear clinically sound and rebounded that develop neonatal seizures and get diagnosed with HIE after an initial window.
Other non-HIE causes of neonatal encephalopathy can be caused by genetic conditions, metabolic disorders, neonatal stroke, or maternal & perinatal infections. HIE can also happen with the other causes of NE, too, and “co-occur”. HIE may be difficult to give a confirmed diagnosis in the first few hours or days, but it is more clearly understood as imaging, clinical presentation, etc. are understood. HIE is still a diagnosis even if a baby or child has a clear MRI. Doctors may want to do additional rule out testing for genetic conditions that can sometimes mirror HIE, and lead to targeted treatments.
Different alternate diagnoses include perinatal encephalopathy, perinatal depression, perinatal asphyxia, neonatal encephalopathy or birth asphyxia.
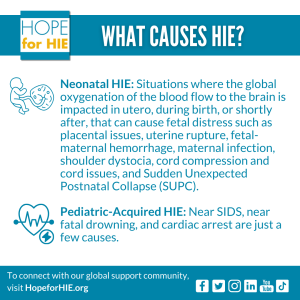
What causes HIE?
HIE is considered “heterogeneous”, meaning there are MANY causes to the cause! These can be during gestation, during the birthing process, after birth, or in childhood.
How is HIE diagnosed?
Diagnosis of HIE in a newborn baby is made using a few different diagnostic tools, in combination. Physical exam, APGAR scores, the Sarnat Scale, which is based upon how the baby appears after birth or injury, and presentation at the hospital, in addition to diagnostic tools and imaging such as EEG, ultrasound and MRI, and checking cord blood gas levels.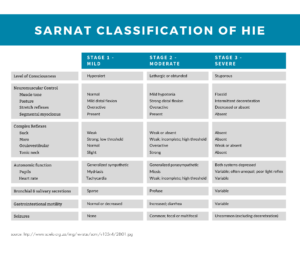
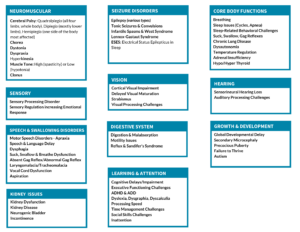
The baby or child may present with the following symptoms:
Treatment
Depending on certain criteria, therapeutic hypothermia, or cooling, has been shown to reduce death and disability in many cases. The cooling treatment is the most widely known and used treatment, but there are other treatments being trialed around the world. It is currently the only approved therapeutic for neonatal HIE, and has been shown ineffective for pediatric-acquired HIE. Cooling can be done on the whole body, or through a cooling cap placed on the head. The baby may also need other medical intervention to support their organs or to treat seizures as they recover.
You can learn more about the research being done to accelerate new therapeutic interventions for HIE on our Clinical Trial & Research Hub.
Babies and children who experience HIE may qualify for early intervention therapy services, after discharge, such as physical therapy, occupational therapy, speech therapy, feeding and swallowing therapy, vision therapy and more.
How many babies are diagnosed with HIE?
About two to three in every 1,000 full-term births in high income countries and 10-30 per 1,000 live births in low and middle income countries will be affected by HIE every year, which means hundreds of thousands of babies and children experience HIE every year. Neonatal encephalopathy, which HIE is the leading cause of, is the 2nd leading cause of infant mortality and lifelong disability worldwide. We are on a mission to ensure none of their families face HIE alone, and to improve the quality of life for this community.
Levels of HIE Explained
The outcomes of children with HIE are wide-ranging – anywhere from unaffected through loss. No two children will be the same, even with a similar injury pattern. The impact of each child’s injury is different based on multiple factors, including what parts of the brain were affected and how damaging the insult was to the brain, and how each child’s brain moves forward from injury through neuroplasticity.
Connect with families, read inspiring stories, and get helpful resources delivered right to your inbox.